Blog Post List

Dental Opioid Prescriptions May Increase Risk Of Subsequent Abuse, Study Suggests.
The Washington Post (12/3, Cohen) reports a studypublished in JAMA Internal Medicine found that “nearly 6 percent of almost 15,000 people between 16 and 25 years old who received initial opioid prescriptions in 2015 from dentists were diagnosed with opioid abuse within a year.” In comparison, the researchers found that “0.4 percent in a similar group who didn’t get dental opioids were diagnosed with opioid abuse during the same period.” The article notes a “study in The Journal of the American Dental Association found that anti-inflammatory analgesics, such as ibuprofen and acetaminophen, generally work better than opioids at easing acute dental pain.” Follow all of the ADA’s advocacy efforts on opioids at ADA.org/opioids. As a public service, the ADA Center for Professional Success website is now offering free access to information on safe prescribing, online continuing education, and other tools for managing dental pain, especially for patients who are at risk for drug overdose or addiction. For more information, visit Success. ADA.org/opioids.
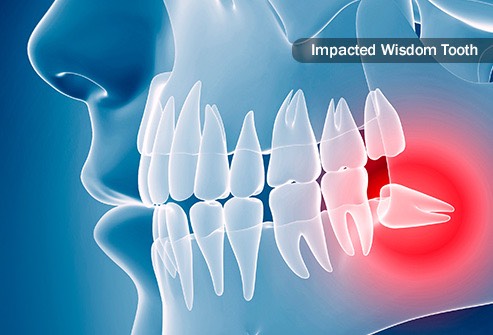
Wisdom Teeth Removal: What You Can Expect
Just the phrase "wisdom teeth removal" is enough to make your mouth hurt, but do you actually know what to expect during and after the procedure? Taking the time to learn more about it can reduce anxiety and help you better prepare for recovery.Regardless of whether you're getting some or all of your wisdom teeth removed, the information below will give you an inside look into what you can expect from the extraction procedure and healing process.What to Expect During the Procedure from your Nashville TN Dentist Depending on how many teeth you're having extracted as well as your comfort level with the procedure, there are different types of anesthesia the oral surgeon might administer:• Local Anesthesia — Administered near the site of each extraction to numb the surrounding area, meaning you're awake during the procedure. While you won't feel pain, you will likely feel pressure and movement.• Oral Conscious Sedation Anesthesia — Administered through medication taken by mouth. During the procedure, you'll be conscious but won't feel pain and will have only some memory of the procedure.• General Anesthesia — Administered through your nose, as an IV line in your arm, or both. You'll be completely unconscious during the procedure and won't remember the surgery.The extraction procedure itself involves several steps. Your Nashville TN Dentist will:• Create an incision to reveal the tooth and bone for removal• Divide the tooth into sections (if necessary) to remove it• Remove the tooth and clean the area where it was of any remaining debris• Stitch the wound closed (in most cases)• Insert gauze over each extraction site to control bleeding and promote clotting. What to Expect After the Procedure from your Nashville TN Dentist. The recovery process is different for every individual and will also vary depending on the type of anesthesia used. Those who receive sedation or general anesthesia will need more time to recover than those who receive local anesthesia.Following these recommendations can promote healing after the procedure:• Bite on Gauze — To control and reduce bleeding, gently bite on gauze pads and be sure to change them about every 20 minutes or so.• Stay Elevated — Prop up the head to reduce bleeding. Laying flat can prolong it.• Apply Ice — During the first 24 hours, applying ice to the outside of the cheek for 15 to 20 minutes at a time will help reduce swelling and bruising.• Rest — Physical activity can exacerbate bleeding, making it important to rest as much as possible and avoid exercise immediately after the procedure.• Eat Soft Foods — Soft foods will be gentle on the areas that were treated, making irritation less likely. Soup, applesauce, and yogurt are great options. Avoid drinking out of a straw, as it can cause the clot to be removed and result in complications.• Keep Your Mouth Clean — After 24 hours, brushing teeth is ok. However, it is important to be careful around the extraction sites. Additionally, the mouth should be rinsed with warm salt water every two hours to clean the wounds.• Don't Smoke — For those who smoke, it is important to refrain for at least 24 hours after surgery.Diminish Fear by Understanding What to Expect, Please ask your Nashville TN Dentist. For many, wisdom teeth extraction is frightening and the recovery process can be just as anxiety inducing. However, by taking the time to understand what happens during and after the procedure, you can ease your concerns and learn how to properly care for yourself and heal as quickly as possible. Sources:Wisdom Tooth Extraction. (2013, August 19). Retrieved June 3, 2014 from http://www.webmd.com/oral-health/wisdom-tooth-extraction. Wisdom Tooth Extraction: What you can expect. (2015, March 31). Retrieved June 3, 2015 from http://www.mayoclinic.org/tests-procedures/wisdom-tooth-extraction/basics/what-you-can-expect/prc-20020652
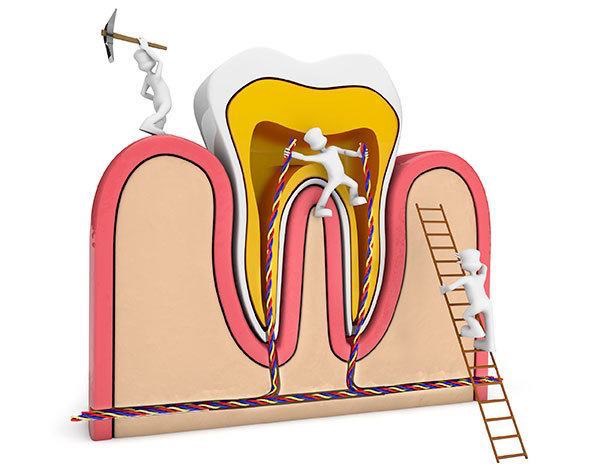
In Defense of Root Canals: The Unsung Hero of Dental Care
Think you might need a root canal? It's not the end of the world, nor is it as torturous as you might think! Even though a root canal is usually the last resort for decayed teeth, when compared with other alternatives, it's quite practical and cost-effective.
Put your fears to rest by discovering the truth about this much-maligned treatment, and find out why it's considered by many dentists to be the unsung hero of dental care.
When and Why Root Canals Are Necessary
Left untreated, tooth decay can eventually result in bacteria infiltrating the very core of the tooth, infecting its sensitive nerve tissue (otherwise referred to as "root" or "pulp"). Once the pulp has been infected, a pocket of pus known as an abscess can form and wreak havoc beyond the problem tooth itself. From swelling of the mouth, jaw and face, to bone loss and even the spread of infection into the skin, the cost of delaying treatment can compound rather quickly.
If the problem is caught in time, a root canal may be possible, allowing the dentist to clear the infected pulp without having to sacrifice the whole tooth. Keeping your natural tooth not only helps maintain proper chewing and speech, but also it requires less time and money compared to a tooth removal and implant.
Signs You Need a Root Canal
If you experience any of these symptoms, you might need a root canal:
Acute, shooting pain when pressure is applied to a tooth. Noticeable darkening or discoloration of the tooth compared to neighboring teeth. Lingering tooth sensitivity, particularly to extremely hot or cold foods. A pimple on the gums that never seems to go away. Swelling of the gums near the problem tooth. Continuous pain or throbbing even when not chewing or using the tooth. See your dentist to know for sure, and let him or her know about your situation when scheduling an appointment to ensure you are seen as soon as possible. Like most dental problems, it's best to be proactive. The sooner the dentist is able to diagnose and treat the infected area the better — and it could decrease the amount of post procedure discomfort.
What to Expect During a Root Canal
The length of time for treatment can vary widely depending on the complexity of each patient's situation, but it's safe to say that multiple visits are required to complete a root canal. Anesthesia may be applied, but it is not always necessary since the nerve is already dead. The first phase of a root canal involves thoroughly ridding the tooth of any infection and decayed matter — usually by drilling an access hole, flushing out the pulp, and applying medication to the tooth and surrounding gums. The dentist will then seal off the area completely, or in extreme cases, wait several days for the infection to clear before sealing off the tooth.
The second phase of treatment focuses on filling the tooth. To do this, a dentist normally uses sealer paste or a rubber-like compound to fill the empty nerve canal and interior of the tooth. After the tooth has been filled, a metal post is inserted into the tooth to further strengthen it.
Restoration, in which a crown is created to cap off the tooth, is the final step of treatment. Once the custom crown arrives, the dentist covers the tooth and shapes the crown to function as optimally as possible.
Post Treatment Care
As with any lengthy dental procedure, temporary tooth and gum sensitivity are to be expected, but should go away within a day or two. If the permanent crown has been applied, you can return back to your normal routine immediately.
Root canals have a very high success rate, but it's important to remember that there is always a possibility for the filling to become infected. To avoid complications and additional root canals down the road, make oral hygiene a top priority and schedule regular visits to your dentist.
Sources:Dental Health and Root Canals. (2015, January 26). Retrieved May 25, 2015 from http://www.webmd.com/oral-health/guide/dental-root-canalsJohnstone, G. (n.d.). The Latest on Root Canals. Retrieved May 24, 2015 from http://www.yourdentistryguide.com/root-canals/What is Root Canal Treatment and Why Would You Want It? (2010). Retrieved May 24, 2015 from http://www.dentalfearcentral.org/faq/root-canal/

Receding Gums: Are Your Teeth in Peril?
No cavities, no problem, right? Wrong! Even the straightest and whitest of teeth can fall prey to a serious case of receding gums, a common condition that can sneak up and do some damage before many individuals realize it's even a problem.While a surefire way to detect and treat it is with regular visits to the dentist, meticulous at-home monitoring and preventative care is also a great line of defense. Here's what you should know to keep the threat of gum recession at bay.Signs and Symptoms of Receding Gums. Gums don't recede overnight, but if you pay close attention, you can spot telltale signs of the problem: a tooth that appears much longer than its neighbors, yellow stains where the tooth touches the gum line, or even a ridge you can feel on the affected tooth, indicating your gums have shifted. Tooth sensitivity is another red flag, as a declining layer of protective gum tissue can leave nerves beneath the enamel exposed.Causes of Receding Gums. Many things can cause vital gum tissue to detach and recede, but the most common culprit is untreated gingivitis. If you have gum disease, chances are that gum recession is just around the corner.Other possible causes include:Brushing too hard, thereby resulting in unnecessary pressure and irritation. Smoking/tobacco use, which can impact blood supply to the gums. Crooked teeth that can pull on the gums, and also lead to gingivitis. Oral piercings that force precious tissue aside over time. Genetics, an inherited predisposition to gum recession. Diabetes, which has been linked to receding gums. Depending on the root cause, the rate of recession may vary, but being aware of all the possible factors can help you steer clear of other hazards and behaviors that will only aggravate the problem.In-Office Treatment Options. The good news is that, if you do have a confirmed case of receding gums, all is not lost. Whether it is mild or extreme, in-office treatments are available to help halt recession — and in some instances, even restore lost tissue.Periodontal therapy is an effective procedure your dentist may recommend to put a stop to further gum erosion. This process involves laser treatments that target and sanitize the problem area(s). With proper care and time, it is possible for the gum tissue to reattach to the tooth's surface.For patients with severe gum recession, the dentist may ultimately advise surgery. Grafting is one common option that may be offered, in which tissue from a donor or another area of your mouth is applied to the affected area. Crown lengthening, or "pocket depth reduction", is another alternative that involves removal of diseased tissue altogether. This treatment may be recommended only if the gums have receded to such a point that tooth loss is imminent, and it can result in tooth sensitivity.Other Steps You Can Take. In addition to seeking professional help, preventative care is critical to combating gum recession. Due to its gradual nature, sometimes a few proactive measures can go a long way:Brush and floss more regularly to help eliminate gum disease. Switch to a soft-bristled toothbrush to apply less pressure on your teeth. Quit smoking/tobacco use to maintain a healthy blood supply to your teeth. Get teeth straightened to help prevent gingivitis, which is linked to receding gums. Use a mouth guard at night to keep teeth grinding from weakening the gums. No matter the source or severity of the problem, see your dentist for help. In addition to the positive impact that regular dental cleanings can have on your gum health, your dentist can craft the optimal treatment plan based on your individual situation.
Sources:Receding Gums. (2014, September 12). Retrieved June 12, 2015, from http://www.webmd.boots.com/oral-health/guide/receding-gumsReceding Gums Causes, Symptoms, Treatment and Prevention.(2014, March 18). Retrieved June 12, 2015, from http://ultrablubrush.com/receding-gums-causes-symptoms-treatment

Have A Heart Problem? 9 Issues Your Dentist Needs To Know About
Heading to the dentist's office with a heart-related issue? It's important to tell your dentist about it! Your mouth and heart are linked in more ways than you might expect – and failing to inform him or her about cardiovascular problems could spell serious trouble. For your health and safety, be sure to let your dentist know if any of the below heart conditions apply to you.
1. Born or Developed Heart Ailments
Any heart ailment – whether past or present – should be discussed with your dentist. Many heart conditions, especially those involving the valves, come with a higher risk for a heart infection, or endocarditis. To prevent harmful oral bacteria from entering the bloodstream, your dentist may find it necessary to place you on antibiotics prior to treatment.
2. High Blood Pressure
Hypertension may cause faintness in the dentist's chair and also exclude you from certain procedures. To ensure that dental work isn't causing any negative effects, your dentist may monitor your blood pressure before and during treatment. In addition, he or she will check for excess gum growth, dry mouth and taste loss – all common side effects of blood pressure medication.
3. High Cholesterol
Similar to hypertension, high cholesterol can also cause light-headedness after being seated in a reclined position. If your dentist is aware of this, he or she can make adjustments to minimize your discomfort. Your treatment plan may also be altered to avoid complications between your cholesterol medication and any medicine your dentist prescribes.
4. Heart Attack
All dental work must be held off for six months after a heart attack, and future treatment will require your dentist to consult with your physician. Because anti-coagulants, a common medication for those who have suffered a heart attack, can prevent blood from clotting, certain procedures or surgeries may require you to stop using the medicine beforehand.
5. Angina
Often characterized as intense pain in the chest, attacks can be triggered both by dental anxiety and certain dental procedures. Your dentist may call for nitroglycerin and oxygen during treatment, as well as blood pressure monitoring. If you take calcium channel blockers to combat angina, he or she may also advise more frequent checkups to monitor for gum overgrowth.
6. Stroke
Blood thinners are often used by stroke survivors, and may interfere with dental procedures. Blood work and a consultation with the physician will be necessary before undergoing any treatment. Because paralysis is a common outcome of a stroke, the dentist may also recommend more frequent visits and different dental products and techniques to maintain proper hygiene.
7. Use of a Pacemaker
Dental work should be avoided for a few weeks after implantation of a pacemaker. Afterwards, treatment can proceed, but it is critical to check with the doctor and even the pacemaker manufacturer for any potential electromagnetic interference that could be caused by common dental devices.
8. Congestive Heart Failure (CHF)
In minor cases, CHF patients may experience dry mouth due to their heart medications, and your dentist may prescribe an oral rinse and suggest certain habit modifications to combat the problem. In severe cases, CHF patients may experience serious complications if seated in a reclined position. Depending on the severity of the condition, it may be necessary for dental work to be completed in a hospital setting.
9. Coronary Artery Bypass Grafting (CABG)
While CABG may not have oral health implications, and antibiotics are usually not necessary before dental work is conducted, severe pain due to this surgery may be experienced when seated in a reclined position. Unless it is an emergency, wait six months before proceeding with any serious dental treatment.
Preventative Care is Paramount
Heart conditions – even those that have been corrected – can have a lasting impact on dental care, so stepping up efforts to prevent dental problems from happening in the first place is even more critical to maintaining good oral health. Consult with your dentist about necessary changes both to your checkup schedule and at-home routine to help keep dental issues at bay.
Sources:
Cardiovascular Diseases. (2013, March 1). Retrieved July 21, 2015, from http://www.colgate.com/app/CP/US/EN/OC/Information/Articles/Oral-and-Dental-Health-Basics/Medical-Conditions/Heart-Disease-and-Oral-Health/article/Cardiovascular.cvsp

What do we know about E-Cigarettes?
What is an e-cigarette? An e-cigarette is a battery-operated device or ‘cigarette’, that delivers flavored nicotine using vapors instead of smoke. The device uses a power source (e.g. lithium ion battery) to heat a metal element. The element aerosolizes the flavored e-liquids, and the user inhales the resulting aerosol. First generation e-cigarettes resemble a cigarette, usually are disposable and readily available at U.S. convenience stores, shopping malls, and gas stations. The latest e-cigarettes use a sub-ohm heating element (more power), replaceable atomizer (convenient) and refillable reservoir (customizable). Most e-cigarettes are imported from China which is the largest manufacturer of e-cigarettes, producing 95% of the world’s e-cigarettes, primarily for the U.S. and the European consumer markets. Electronic cigarettes. 1: first generation e-cigarette, 2: second generation e-cigarette (AKA tank system), 3: latest generation e-cigarette (AKA sub-ohm system), 4: heating elements, 5: e-cigarette power delivery system, and 6: e-liquid Reference Material (RM). What is e-liquid? Most e-liquids contain four base chemicals: propylene glycol, vegetable glycerin, nicotine, and flavoring(s). In the U.S., over 400 companies distribute thousands of e-liquids through local ‘vape shops’ and online stores. 1 In 2014, there were over 7,700 different e-liquid formulations available on the market and it is estimated that more than 200 new flavors are being introduced monthly.1 Quality control and industry standards for e-liquid manufacturing process are not yet fully implemented. Thus, there are significant product and batch variations; and impurities are commonly found in consumer products. 2-12 The lack of child-proof containers poses a serious threat to infants and toddlers. Sophisticated packaging for candy-flavored e-liquids, which targets youth, can be indistinguishable from real candies which, in part, is responsible for accidental ingestion. The American Association of Poison Control Centers (AAPCC) receives on average 10 calls a day from people regarding children who were accidentally exposed to e-cigarette devices and liquid nicotine.13 E-liquids. ~10,000 e-liquid formulations are available from local vape shops and online stores in U.S. (credits: www.vaporhq.com, www.vape.deals.com, www.vaportrim.com, www.flavors.com, and www.skittlesejuice.com). What are the potential dangers/risks of using e-cigarettes? Chemical analyses of e-cigarette aerosol: We found that three factors could significantly impact research outcomes: (1) types of e-cigarette devices (e.g. ecigarette generation and design) used in the study, (2) the amount of power (in wattage) delivered to the system, and (3) composition of e-liquids aerosolized (specifically the types of flavorings used). A consensus on e-cigarette testing standards from the industry, government agencies and academia would be necessary prior to putting the chemical analysis into perspective and to better assess potential health dangers and risks associated with e-cigarette usage. Youth: Currently we do not have long-term data to understand the physiological, psychological, and developmental effects of e-cigarette on youth. Some researchers consider e-cigarettes as ‘gateway devices,’ in that kids are introduced to tobacco products via vaping and once addicted to nicotine, ‘graduate’ to traditional products such as cigarettes, cigars, chewing tobacco and hookah. 14,15 Although the complexity of youth’s vaping/smoking behavior remains to be seen, it is certain that e-cigarette products are easier for children to obtain compared to regular tobacco products.16 Studies show e-cigarettes have surpassed combustible cigarettes as the most commonly used tobacco product among middle school and high school students.17-19 Marketing, internet availability and sweet flavorings may have contributed to this shift. In a 2016 report, the U.S. Surgeon General states that e-cigarette usage among youth and young adults has become a public health concern. 20 Regardless of how nicotine is delivered (by e-cigarettes or combustible cigarettes), nicotine negatively affects adolescence brain developmental processes and may lead to psychiatric disorders and cognitive impairment in later life. 20,21 This report and ongoing research will clarify the public’s perceived safety of e-cigarettes in the future. 4 CDC Morbidity and Mortality Weekly Report (MMWR). A simple and effective message to raise public awareness of e-cigarettes’ potential risks (credit: www.cdc.gov/mmwr/). 5 Devices: According to the latest FDA study, since 2009 there have been 92 overheating, fire and explosion cases involving e-cigarette devices in the U.S.22 Forty-seven people were injured and 67 cases involved property damage. Injuries overall included chemical and thermal burns, smoke inhalation, fractured neck vertebrae, fractured palate and finger loss, displacement or damage of one or more teeth, lacerations, bruising, psychological distress, sensory disturbances, nicotine overdose and oral discolorations. 22 The causes of the device failures are incompletely defined. However, many of the fire and explosion cases occurred while charging lithium batteries in e-cigarettes. Potential explanations of the fires and explosions may include: (1) user error, (2) lack of a clear charging instruction, (3) faulty charging units, (4) lack of overcharge protection / automatic built-in shut off switch, (5) substandard lithium ion batteries, and (6) counterfeit e-cigarette devices and lithium ion batteries. Counterfeit lithium ion batteries. Substandard, potentially dangerous lithium ion batteries are available from online retail stores. Some counterfeit batteries are so sophisticated that it is almost impossible to distinguish from genuine products by a visual inspection (credit: www.tasteyourjuice.com). Who regulates e-cigarettes and e-liquids? Effective August 8, 2016, U.S. Food and Drug Administration (FDA) regulates ecigarettes under the “Deeming Tobacco Products Amendment” (Docket No. FDA2014-N-0189). The new rule extends the FDA’s regulatory authority to all tobacco products, including e-cigarettes, cigars, hookah (AKA waterpipe tobacco), pipe tobacco, nicotine gels, and dissolvables.23 The FDA expects, by 2019, the new regulation will be fully implemented and enforced. The FDA states the rule will help prevent young people from starting to use these products, help consumers better understand the risks of using these products, prohibit false and misleading product claims, and prevent new tobacco products from being marketed unless a manufacturer demonstrates that the products meet the relevant public health standard.23 The new rule is well-received and welcomed by most U.S. health care professionals and organizations. FDA’s new regulations. FDA finalized a rule that extends its regulatory authority to all tobacco products, including e-cigarettes, cigars, and hookah and pipe tobacco, as part of its goal to improve public health (credit: www.fda.org). What are the challenges associated with e-cigarette research? A major challenge in e-cigarette research is that there is no scientific consensus. Misleading, inconsistent and contradictory research findings have polarized scientists, policy makers and the public, leaving them with few scientific facts to evaluate potential risks of using e-cigarettes. Many contributing factors to the inconsistent and contradicting findings include lack of standardized research materials, testing devices and test methods.24 Several studies in the early phase of e-cigarette research have been financially supported by e-cigarette companies. Although the funding sources were fully disclosed, some scientists still raised their concerns regarding implied conflict of interest. In contrast, various vaping advocacy associations have pointed out that some published studies used unrealistic power settings (e.g. extremely high voltage) to generate carcinogens such as formaldehyde and other toxins in the aerosol.25-28 Whether the researchers intentionally operated the e-cigarettes to produce hazardous chemical byproducts to inflate the potential danger of e-cigarettes or they mistakenly used the high voltage due to lack of experience in using the device is up for a debate. Considering there are close to 10,000 different e-liquid formulations and hundreds of e-cigarette devices, many with significant quality variations, it is difficult for researchers to keep up with vast array of products in the e-cigarette consumer market and the rapid changes in e-cigarette technology.24 Mutually agreed research materials, testing devices and test methods are needed to bring clarity to the current situation. How can a Reference Material (RM) help the e-cigarette research? The challenges of product testing, quality control and quality maintenance are not new to the manufacturing industry. Manufacturers have applied various quality control practices to improve the manufacturing process and product quality. One of the most common methods is implementing a Reference Material (RM) in the quality control process. RM is a matrix-matched material with assigned target values and assigned ranges for each variable, reliably determined from data obtained by repeated analysis. 29 RMs are routinely used to check the quality and metrological traceability of products, as well as for instrument calibration. The Reference Cigarettes produced by the Center for Tobacco Reference Products (University of Kentucky), for example, have provided much needed standards for tobacco manufacturers, government agencies and research institutions. Although the Reference Cigarettes are different from consumer cigarettes (e.g. Marlboro, Lorillard, or Camel), the Reference Cigarettes come with well-characterized and traceable physical properties. Researchers and manufacturers can use them as a consistent baseline or as a control to compare and characterize new products. Scientists at the ADAF Volpe Research Center recently developed three Reference Materials for e-liquid standards.24 When used appropriately, the reference e-liquids can serve as a control in research experiments and during the manufacturing processes. Reference Material (RM). Implementation of a Reference Material improves product quality for manufacturers and provides research standards for researchers. Where can I get more information about the latest e-cigarette research and reference e-liquid? The latest e-cigarette research information can be found from the following peerreviewed journals: Tobacco Induced Diseases: https://tobaccoinduceddiseases.biomedcentral.com/ Tobacco Control: http://tobaccocontrol.bmj.com/ Nicotine and Tobacco Research: https://academic.oup.com/ntr More information on the research grade reference e-liquid can be found here: http://rdcu.be/pkoz and, by contacting Dr. Jeffrey Kim directly at: E-Liquid Reference Material. The reference e-liquid can be used to check the quality and metrological traceability of commercial e-liquids during a pre-market testing period, instrument calibration, toxicological risk assessment, and safety and efficacy of e-cigarette devices. References 1. Zhu SH, Sun JY, Bonnevie E, et al. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23 Suppl 3:iii3- 9. 2. Brown CJ, Cheng JM. Electronic cigarettes: product characterisation and design considerations. Tob Control. 2014;23 Suppl 2:ii4-10. 3. Callahan-Lyon P. Electronic cigarettes: human health effects. Tob Control. 2014;23 Suppl 2:ii36-40. 4. Orr MS. Electronic cigarettes in the USA: a summary of available toxicology data and suggestions for the future. Tob Control. 2014;23 Suppl 2:ii18-22. 5. Goniewicz ML, Kuma T, Gawron M, Knysak J, Kosmider L. Nicotine levels in electronic cigarettes. Nicotine Tob Res. 2013;15(1):158-166. 6. Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133-139. 7. Hutzler C, Paschke M, Kruschinski S, Henkler F, Hahn J, Luch A. Chemical hazards present in liquids and vapors of electronic cigarettes. Arch Toxicol. 2014;88(7):1295- 1308. 8. Cobb NK, Byron MJ, Abrams DB, Shields PG. Novel nicotine delivery systems and public health: the rise of the "e-cigarette". Am J Public Health. 2010;100(12):2340- 2342. 9. Cameron JM, Howell DN, White JR, Andrenyak DM, Layton ME, Roll JM. Variable and potentially fatal amounts of nicotine in e-cigarette nicotine solutions. Tob Control. 2014;23(1):77-78. 10. Cheah NP, Chong NW, Tan J, Morsed FA, Yee SK. Electronic nicotine delivery systems: regulatory and safety challenges: Singapore perspective. Tob Control. 2014;23(2):119-125. 11. Etter JF, Zather E, Svensson S. Analysis of refill liquids for electronic cigarettes. Addiction. 2013;108(9):1671-1679. 12. Hadwiger ME, Trehy ML, Ye W, Moore T, Allgire J, Westenberger B. Identification of amino-tadalafil and rimonabant in electronic cigarette products using high pressure liquid chromatography with diode array and tandem mass spectrometric detection. J Chromatogr A. 2010;1217(48):7547-7555. 13. http://www.aapcc.org/alerts/e-cigarettes/ 11 14. Barrington-Trimis JL, Berhane K, Unger JB, et al. The E-cigarette Social Environment, E-cigarette Use, and Susceptibility to Cigarette Smoking. J Adolesc Health. 2016;59(1):75-80. 15. Barrington-Trimis JL, Urman R, Berhane K, et al. E-Cigarettes and Future Cigarette Use. Pediatrics. 2016;138(1). 16. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6349a1.htm 17. https://www.cdc.gov/mmwr/volumes/65/wr/mm6514a1.htm 18. https://www.drugabuse.gov/trends-statistics/monitoring-future/monitoring-futurestudy-trends-in-prevalence-various-drugs 19. https://www.cdc.gov/mmwr/volumes/65/wr/mm655051a2.htm 20. https://www.surgeongeneral.gov/library/2016ecigarettes/index.html 21. https://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf 22. Rudy SF, Durmowicz EL. Electronic nicotine delivery systems: overheating, fires and explosions. Tob Control. 2016. 23. http://www.fda.gov/TobaccoProducts/Labeling/RulesRegulationsGuidance/ucm 32094909.htm 24. Kim JJ, Sabatelli N, Tutak W, et al. Universal electronic-cigarette test: physiochemical characterization of reference e-liquid. Tob Induc Dis. 2017;15:14. 25. Sodhi SK, Khanna A. More on hidden formaldehyde in e-cigarette aerosols. N Engl J Med. 2015;372(16):1576. 26. Thomson RH, Lewis PM. More on hidden formaldehyde in e-cigarette aerosols. N Engl J Med. 2015;372(16):1575-1576. 27. Nitzkin JL, Farsalinos K, Siegel M. More on hidden formaldehyde in e-cigarette aerosols. N Engl J Med. 2015;372(16):1575. 28. Pankow JF, Strongin RM, Peyton DH. More on hidden formaldehyde in e-cigarette aerosols. N Engl J Med. 2015;372(16):1576-1577. 29. http://www.who.int/water_sanitation_health/resourcesquality/wqmchap6.pdf?ua=1

The Mouthwash Mistake You Could Be Making
It can freshen up your breath faster than brushing, but does mouthwash really make a big difference when it comes to your oral health? You may be surprised to find that looks–or in this case, smells–can be deceiving! Oral rinses are not created equal, and if you're not careful, some can actually be more harmful than helpful. Find out whether your go-to for gargling is doing you any good, or if another mouthwash makes sense for you.
Therapeutic vs. Cosmetic Mouthwashes
Most mouthwashes claim to eliminate bad breath, but how they go about doing this can differ significantly. In general, over-the-counter oral rinses fall into two categories:
"Therapeutic" Mouthwashes. Comprised of various anti-microbial agents, these mouthwashes have plaque-fighting properties that can give your oral hygiene an added boost by inhibiting the growth of oral bacteria. Oftentimes, they may be further enhanced with fluoride to help combat tooth decay. Therapeutic mouthwashes proven to treat the root causes of bad breath are easy to tell apart from other mouthwashes because they come with an ADA seal of approval. In some cases, a special type of therapeutic rinse may be prescribed by your dentist.
"Cosmetic" Mouthwashes. Similar in appearance to therapeutic mouthwashes, cosmetic rinses also promise to control bad breath, but a closer look at the label will reveal both the lack of active ingredients and an ADA seal of approval. This means that while your breath may smell fresher, the mouthwash only serves to temporarily mask the odor, and doesn't specifically attack oral bacteria or built-up plaque.
If you've reviewed the product details carefully, but are still unsure whether your mouthwash is therapeutic or cosmetic, call your dentist for confirmation. He or she can easily verify its safety and effectiveness.
Choosing the Right Mouthwash
With countless options available, choosing mouthwash can be overwhelming, but a simple self-assessment is an easy way to narrow down the field:
If your breath is normally fresh...A cosmetic rinse might be right for you. Keep a travel-sized bottle on hand for occasional use if/when your breath feels stale or smells bad due to something you may have eaten.
If you have chronic bad breath (or "halitosis")...See your dentist first. He or she can determine the severity and likely causes, and advise whether the best solution can be found over-the-counter or if a prescription rinse is necessary. Either way, a therapeutic rinse will be most beneficial to keep bacteria at bay and help resolve your bad breath problem permanently.
If you have other dental problems in addition to bad breath...Look for therapeutic rinses that come with added benefits. Those who have trouble with tooth decay, for instance, may fare better with a cavity-fighting mouthwash enriched with fluoride. Others who struggle with dry mouth ("xerostomia"), burning mouth syndrome, or have noticed an adverse reaction to traditional rinses, on the other hand, should reach for a non-aggravating, alcohol-free rinse. Nowadays, mouthwashes come with different benefits to meet varying preferences and dental goals: from those with whitening ingredients to organic mouthwashes and beyond.
Brushing and Flossing Always Come First
No matter which rinse you choose, it's important to remember that mouthwash is only meant to supplement–not substitute for–brushing and flossing. Ultimately, the best way to get rid of the bacteria and plaque that cause bad breath in the first place is with good oral hygiene and regular visits to the dentist's office. To ensure your at-home routine is meeting your dental needs, be sure to share your hygiene practices and products with your dentist.
Sources:
Benefits and Risks of Mouthwash. (2013). Retrieved June 10, 2015, from http://oralhealth.deltadental.com/Adolescent/BadBreath/22,21555
How to Use Mouthwash. (n.d.) Retrieved June 5, 2015, from http://www.wikihow.com/Use-Mouthwash
Learn More About Mouthwash. (2015). Retrieved June 10, 2015 from http://www.ada.org/en/science-research/ada-seal-of-acceptance/product-category-information/mouthrinses